Understanding Nasal Polyps
Nasal polyps are abnormal, soft growths in the nose or sinuses. They are swollen bulbs of inflamed tissue along the nasal lining. Anyone can develop nasal polyps. However, they are more common in people with asthma and people 40 to60 years old.
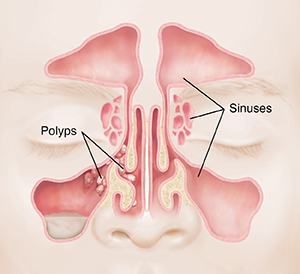
How polyps affect the sinuses and nasal cavity
The sinuses are a group of air-filled spaces formed by the bones of your face. They connect with the nasal cavity. This is the large space behind your nose. Normally, all of these spaces are fairly open and air flows freely. But nasal polyps can grow and block the space. This can make it hard to breathe through your nose.
Nasal polyps may be a result of ongoing (chronic) rhinosinusitis. This is a condition in which the nasal cavity and sinuses are inflamed for 12 weeks or longer. However, not all people with this condition will develop nasal polyps.
What causes nasal polyps?
Researchers are still learning about the causes of nasal polyps. Inflammation of your nasal tissue is part of the cause. Nasal polyps are more common in people with health conditions such as:
Certain genes may also cause nasal polyps to grow. This includes genes that play a role in your immune system and inflammatory response. You may be more likely to develop nasal polyps if other members of your family have had them.
Symptoms of nasal polyps
If you have nasal polyps, you may feel like you have a cold for months or longer. Some of your symptoms may be due to nasal polyps. Others may result from the chronic rhinosinusitis that caused your polyps.
The most common symptoms of nasal polyps include:
-
Stuffy nose (nasal congestion)
-
Runny nose
-
Feeling of fullness in your facial sinus, but often not pain
-
Postnasal drip
-
Reduced smell
-
Feeling blocked in your nose and needing to breathe through your mouth
Diagnosing nasal polyps
Your healthcare provider will ask about your health history and symptoms. They will look inside your nose with a lighted tool. The polyps may be seen with this simple exam. Your provider may refer you to an ear, nose, and throat specialist (ENT or otolaryngologist).
Your healthcare provider might need more information about your sinuses and nasal cavity. They may want to diagnose the trigger of your polyps, such as allergies. You may need tests such as:
-
Nasal endoscopy. This looks more closely at your inner nose and your sinuses. It is done with a thin, flexible tube with a light and camera on the end. It’s put into your nose to give a detailed view of your polyps.
-
CT scan. This imaging test is done if the diagnosis isn’t clear. X-rays pass through your nose and create detailed images that are put together by a computer.
-
MRI. This imaging test may be done if needed. It uses strong magnets to create an image of tissues inside your body without the use of X-rays.
-
Allergy testing. This is done to diagnose allergies.
-
Other tests. Tests may be done to diagnose the airflow in the nasal cavity.
-
Polyp biopsy. This is done if needed to rule out cancer. A polyp or small piece of a polyp is removed and checked for cancer cells.
Treating nasal polyps
Your healthcare provider may recommend treatment for your nasal polyps. The treatment will depend on the number and size of the nasal polyps. Treatment may include:
-
Corticosteroids. You may receive these medicines as pills or in a nasal spray.
-
Surgery. Surgery may be needed if the polyps block your airways or cause frequent sinus infections.
-
Biologics. These medicines are injected under the skin and may need to be taken long-term.
Nasal polyps may come back if the underlying irritation or allergy isn't addressed. Talk with your healthcare provider about what treatment options are right for you.