Breast Lift or Implants
A breast lift (mastopexy) and breast implants (augmentation) are cosmetic surgeries that change the look and size of the breasts. A breast lift helps reshape breasts that have lost their firmness and sag or droop. Augmentation involves putting breast implants above or below the chest muscle, to make the breasts larger. Together, these procedures change the look and size of the breasts. This sheet tells you more about these surgeries and what to expect. Sometimes these surgeries are done together. But depending on your body, medical condition, and your health needs, your surgeon may advise 2 separate surgeries. This lets you heal in between.
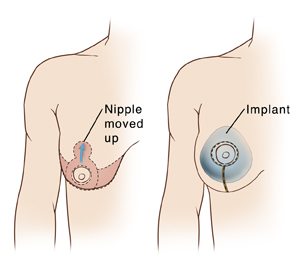 |
| This picture shows one type of mastopexy and possible incision placement. Talk to your surgeon about how your own surgery will be done. |
Different kinds of implants
Breast implants are made of a silicone shell. The shell may be filled with saltwater (saline) or gel (silicone). Different implant sizes, shapes, and textures are available, as well as different thicknesses of silicone filling. There are benefits and drawbacks to each type of implant. You and your surgeon will discuss which type is best for you and your healthcare needs.
Getting ready for surgery
Meet with your surgeon before the day of surgery to ask questions about the surgeon's experience with breast implants, your specific surgery, and the results you can expect. The FDA has a list of questions that may help you. Ask your surgeon what makes you a good candidate for breast implants, and what your choices are for size, shape, and surface texture. Your surgeon will also go over the risks and benefits of each surgery. Ask for before and after pictures of other patients so you can understand if your expectations are realistic.
During this meeting, ask the surgeon for a copy of the patient labeling for the breast implant that will be used. As a patient, it's your right to have this information and the surgeon will expect to provide it. Talk with your surgeon about the risk of breast implant-linked anaplastic large cell lymphoma (BIA-ALCL). This is a rare type of non-Hodgkin's lymphoma that can develop after breast implants. The exact number of cases is not known. But the most current data suggest that BIA-ALCL is seen more often after breast implants or tissue expanders with textured surfaces than those with smooth surfaces.
Read and understand the informed consent form. Ask any questions before you sign it.
Get ready for the surgery as you have been told. In addition:
-
Tell your surgeon if you think you could be pregnant.
-
Tell your surgeon if you are ill.
-
Some surgeons ask that you have a mammogram or breast X-rays before the surgery. This helps show any breast abnormality. And it gives the surgeon a pre-surgery image of your breast tissue.
-
Tell your surgeon about all prescriptions and over-the-counter medicines you take. This also includes vitamins, herbs, and other supplements. It also includes any blood thinners, such as warfarin, certain anti-inflammatory medicines, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery.
-
Follow any directions you are given for not eating or drinking before your surgery. This includes coffee, water, gum, and mints. (If you have been directed to take medicines, take them with a small sip of water.)
-
Don't smoke. Smoking can reduce the blood flow in the skin and increase your risk of wound-healing complications. Your surgeon may delay your surgery if you smoke before surgery. Join a stop-smoking program to improve your chances of success.
The day of surgery
A breast lift with breast implants takes about 3 to 5 hours. You may go home the same day. Or you may stay overnight in a hospital or ambulatory surgical center.
Before the surgery begins
-
An IV (intravenous) line is put into a vein in your arm or hand. This line delivers fluids and medicines.
-
You will be given medicine to keep you pain-free during surgery. This may be general anesthesia, which puts you into a state like deep sleep. A tube may be inserted into your throat to help you breathe. Or you may have sedation, which relaxes you and makes you sleepy. If you have sedation, local anesthesia will be injected to numb the area being worked on. The anesthesiologist will discuss your choices with you.
During the surgery
-
For the breast lift. The surgeon makes incisions in the skin around your breast. You and your surgeon will have discussed incision sites before surgery. The surgeon moves the breast tissue higher on the chest. Breast skin is tightened to hold the tissue in position. Any extra skin is removed. The dark skin around the nipple (areola) and the nipple are moved higher on the breast. If the areola's size is being decreased, skin is removed. The areola is stitched into place. All of this is repeated for the other breast.
-
For the breast augmentation. The surgeon forms a “pocket” to hold the implant. This may be above or below the chest muscle. The surgeon then inserts the implant through the incision and into the pocket. If the implant needs to be filled with saline, that’s done next. The implant is then put in place. If both breasts are being treated, this is all repeated on the other breast.
-
When both stages are done, incisions are closed with stitches, surgical glue, or both. A tube (drain) may be placed into an incision before it is closed. This drains extra fluid that may build up as the wound starts to heal.
After the surgery
You'll be taken to he PACU (postanesthesia care unit) to be watched as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used during surgery, your throat may be sore at first. You'll be given medicine to control pain or nausea. When you’re ready, you can go home with an adult family member or friend. Or you may be taken to a room to stay overnight.
Recovering at home
Once home, follow any directions you are given. Your surgeon will tell you when you can return to your normal routine. During your recovery:
-
Take any prescribed medicines exactly as directed.
-
Wear the special bra or bandage you were given before discharge as directed by your surgeon.
-
Care for your incisions and the bandages as directed by your surgeon.
-
Follow your surgeon’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that could cover the incisions with water until your surgeon says it’s OK.
-
When you shower, gently wash your incision sites. Then pat them dry. Don’t apply lotions, oils, or creams to the incisions until after they are fully healed.
-
Don’t raise your arms above breast level for 10 days, or as directed. And don’t lift, push, or pull anything heavier than 10 pounds for at least 7 days, or as directed.
-
Don’t drive until you are no longer taking prescription pain medicine and your surgeon says it’s OK. When riding in a car, carefully position the seatbelt so that it doesn’t squeeze (compress) your breasts.
-
Breast swelling may last for 3 to 5 weeks. The implant position may change slightly as you heal. If advised by your surgeon, use a cold pack to ease discomfort and control swelling. To make a cold pack, place ice in a plastic bag that seals at the top. Don't put the cold pack directly on the skin. Instead wrap it in a clean, thin towel or cloth. Don't leave the cold pack on for too long, or your skin could be damaged. Put the pack over your bandages for no more than 20 minutes at a time, or as directed. Then leave it off for at least 20 minutes, or as directed. Repeat this as often as needed during waking hours until swelling starts to improve. Don’t fall asleep with the cold pack on. If you’re not sure how to safely use the cold pack, ask your surgeon.
When to call your healthcare provider
Call your surgeon or healthcare provider right away if you have any of the following:
-
Severe swelling in one or both breasts
-
A fever of 100.4°F ( 38°C) or higher, or as directed by your surgeon
-
Bleeding or drainage through the special bra or bandage
-
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, pain that gets worse, or foul-smelling drainage
-
Pain that is not eased by medicine or pain that gets worse
-
More soreness, swelling, or bruising on one breast than the other
-
Breast that is very warm to the touch
Call 911
Call 911 right away if you have:
-
Extreme chest pain
-
Trouble breathing
Follow-up
You will have follow-up visits so your surgeon can see how well you’re healing. If needed, stitches or drains will be removed at one of these visits. If you have any questions about your recovery, let your surgeon know. And tell your surgeon if you notice any changes in your breasts during or after your recovery. This may include injury to the breast or dimpling of the skin of your breast or nipple. If the implants leak or break, they will need to be removed or replaced. Also, be aware that your breasts may sag again over time. If you have any concerns about your surgery results, talk with your surgeon.
Risks and possible complications
Risks and possible complications include:
-
Bleeding or infection
-
Blood clots
-
Capsular contracture (scar tissue squeezing the implant)
-
Breasts that are not the same shape or size
-
Excessive or visible scarring
-
Changes in breast or nipple sensation (temporary or permanent)
-
Rupture or leakage of an implant
-
Persistent pain
-
Wound healing problems or injury to the skin
-
Death of fat cells deep in the skin (fat necrosis)
-
Potential for breasts to sag again
-
Not being happy with cosmetic result
-
Risks of anesthesia