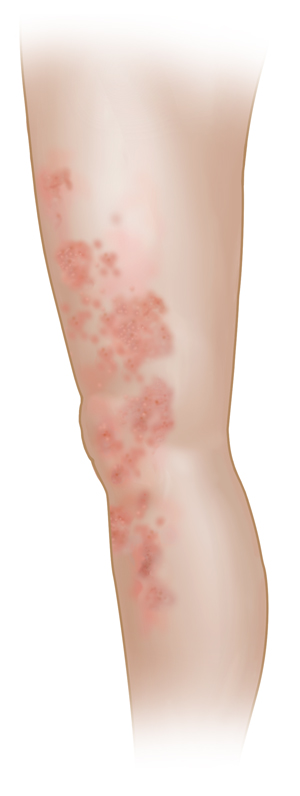
Nonspecific Skin Rash
A rash is a common skin condition. Rashes can be red, itchy, swollen, dry, or painful. You may also have blisters, blotches, or welts on the skin.
A rash can occur for many reasons. And it may go away quickly on its own or with some basic home treatment. Rashes can be hard to diagnose, as they may be caused by many different conditions. But it’s important to get a diagnosis, because some rashes can be a sign of something more serious, or an underlying medical problem.

What causes nonspecific skin rash?
Skin rashes often occur as a reaction to different things. Sometimes the disease-fighting cells (immune cells) in the skin are reacting to an irritant that has touched the skin. These cells may be reacting to an illness or an infection in other cases. Some of the things that can cause a rash to occur include:
-
Skin diseases such as eczema or psoriasis
-
Foods you’re allergic to
-
Medicines you’re allergic to
-
Too much sun exposure
-
Scents in lotions, soaps, laundry detergent, or makeup
-
Some types of fabric or clothing
-
Irritants such as pesticides, paints, and chemicals (strong detergent)
-
Infections caused by a virus (chickenpox), bacteria (strep), or fungus (ringworm)
-
Insect bites
-
Contact with certain plants (poison ivy), or allergy-causing substances such as animal dander or pollen
-
Nickel, a metal often used in inexpensive jewelry and in e-cigarette devices
A rash can sometimes be caused by a health condition such as:
Symptoms of nonspecific skin rash
The symptoms of skin rashes can vary but may include:
Treatment for nonspecific skin rash
Many skin rashes get better with home treatment. Here are some tips:
-
Try an over-the-counter hydrocortisone cream on the affected area if the rash is small.
-
Take an over-the-counter antihistamine to ease itching.
-
Don’t scratch the skin.
-
Wash your skin with mild soap and warm water. Don’t use harsh soaps or scented lotions.
-
Gently pat your skin dry. Don’t rub the skin.
-
Wear cotton clothing.
-
Take a soothing bath with lukewarm water.
Your healthcare provider may prescribe medicines if home treatment doesn’t help:
-
Steroid creams or ointments
-
Anti-inflammatory medicines (corticosteroids) taken by mouth
-
Many other medicines and treatments
When to call your healthcare provider
Call your healthcare provider or seek medical care right away if any of these occur:
-
The rash appears after taking a new medicine.
-
The rash doesn’t go away, or spreads to other areas.
-
You have a rash and a fever of 100.4°F (38°C) or higher, or as advised by your provider.
-
Your child has a rash and a fever (see Fever and children, below).
-
The rash is painful.
-
The rash is on your face or genitals.
-
The rash occurs suddenly and spreads quickly.
-
The rash looks infected. You have swelling, pain, fluid, crusting, or warmth at the rash site. Or you have a red line coming from the rash.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4°F (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older