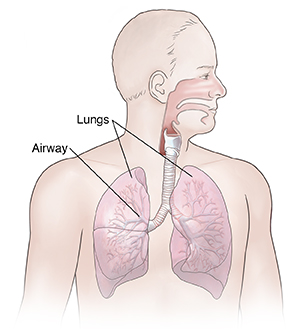
Understanding Bronchial Thermoplasty (BT)
Bronchial thermoplasty (BT) is a treatment for severe asthma. It's FDA-approved for people age 18 and older. BT is most often used in people whose asthma can’t be controlled with medicines. It reduces the amount of smooth muscle that lines the lungs’ airways. This smooth muscle layer is often thicker in people with severe asthma. Reducing it means that the airways don’t get as narrow during an asthma attack. This can reduce the number of severe asthma attacks.
Who should have BT
Your healthcare provider may advise BT if you have severe asthma and:
-
You are between ages 18 and 65
-
Your asthma is not controlled with inhaled medicines (glucocorticoids) or long-acting asthma medicines (beta agonists)
-
You need steroids in pill or liquid form to keep your asthma under control
-
You have not smoked in the past year
You should not have this procedure if you:
-
Have an implantable electronic device, such as a pacemaker
-
Are sensitive to the medicines (sedative and anesthesia) that are used during BT
-
Have other health conditions that may raise the risk for complications
There may be other reasons why you should not have this procedure. Talk with your healthcare provider about any concerns you may have.
Risks of BT
Any procedure has risks. The possible risks of BT include temporary short-term worsening of your breathing problems. This can happen because of irritation of the airways. If this occurs, you may have wheezing, trouble breathing, and a tight feeling in your chest. In rare cases, you may need to be treated in a hospital.
Before the procedure
To get ready for the procedure:
-
Tell your healthcare provider about all the medicines you take. This includes prescription and over-the-counter medicines, vitamins, herbs, and other supplements. You may need to stop taking some or all of these medicines before the procedure.
-
Tell your provider about any recent illnesses, allergies, or health conditions.
-
Follow any directions you are given for not eating or drinking before the procedure.
Follow any other directions you are given before the procedure.
During the procedure
This procedure is done by a lung healthcare provider (pulmonologist) in a hospital. It's done in 3 different sessions. Each session treats a different part of the lungs. You will have about 2 to 3 weeks between each session. No cut (incision) is needed for this procedure. For each treatment session you can expect:
-
First you will have a breathing test (spirometry) to check your lung function.
-
You will be given a steroid pill to help reduce swelling that may occur during the procedure.
-
You will be given medicine by IV (intravenously) to make you sleepy. You may also have medicine to numb your mouth and throat.
-
A thin, flexible tube with a light on the end (bronchoscope) is put into your nose or mouth and moved down into your lungs. A thermoplasty tube is then passed through the scope. It applies heat to the inside of the large airways. This thins the smooth muscle layer.
-
When the procedure is over, both tubes are removed.
-
You will be given another steroid pill to help reduce swelling.
After the procedure
You will be watched for a few hours after the procedure. If your asthma symptoms get worse, you may need to stay in the hospital overnight.
Once you are home, you will follow up with the healthcare provider to see how you are doing. You will also be scheduled for your next BT session.
Note
BT isn’t a cure for asthma. After all of the BT sessions are done, your asthma symptoms may not be as severe. And you may have fewer flareups. But you will still need to take medicines and stay away from triggers to help control asthma.