Your Amputation Surgery
Amputation is a surgery to remove a limb or part of a limb. It's done when tissue in the limb is diseased or damaged and can’t be healed. The surgeon saves as much of your limb as possible. This may include joints, such as the knee. But you may not know before the surgery how much of the limb will remain. Amputation is meant to restore function. Removing your diseased or damaged limb can improve your health. Common causes of amputation include:
Your healthcare provider and team will work with you to set up a treatment plan. Take an active role in your care and ask questions. Ask your healthcare team about anything that isn't clear to you. Here are some questions to ask:
-
How will my pain be managed?
-
How soon will I be able to stand after surgery?
-
Will I get an artificial limb (prosthesis)?
-
Where can I find support after my amputation?
-
When will I start therapy after surgery?
-
When will I be able to go home?
During the surgery
You will most likely get general anesthesia. This will let you sleep comfortably during the surgery.
The surgeon divides damaged tissue from healthy tissue. This includes skin, muscle, bone, blood vessels, and nerves. Then the surgeon removes the damaged part of the limb. The remaining nerves are cut short and allowed to pull back into the healthy tissue. This protects and cushions them.
The end of the cut bone is trimmed and the edges are smoothed for comfort. A flap of healthy muscle and skin is left behind when the damaged tissue is removed. The flap is brought snugly over the bone to cover the end of the amputated limb. If there isn’t enough tissue in the flap, the surgeon takes skin or tissue from some other part of the body. The flap is then stitched or stapled in place.
The wound may be left open at first if debris is present or infection is possible. This lets fluid drain and helps the wound heal cleanly. The wound will later be closed by the surgeon.
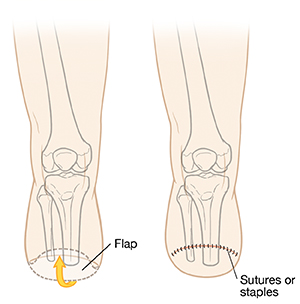 |
| A flap of muscle and skin is brought over the end of the bone and sutured or stapled in place. Location of the sutures or staples vary. |
Risks and possible complications of surgery
-
More surgery needed to remove more of the limb
-
Poor wound healing
-
Infection
-
Severe bleeding
-
Pain, including nerve-related symptoms, chronic pain, and phantom limb pain
-
Blood clots
-
Heart problems (heart attack, arrhythmias, heart failure)
-
Unable to fully straighten the limb
-
Depression
-
Death
After the surgery
Pain management
Your pain will be watched at all stages of your recovery. Talk to your care team about options for medicine and other treatments to help manage your pain. When you wake up after surgery, you’ll have medicine to help keep you comfortable. It will likely be given along with fluids through an IV (intravenous) line that’s placed in a vein. Later, as the pain eases, you’ll take pain pills as needed.
Other care
You’ll have a splint or some other form of pressure dressing on your residual limb. This helps control swelling and aid healing. You may be started on blood thinners to prevent blood clots. You will get antibiotics just before surgery. These may continue after surgery. This is to help prevent infection. You may have a urinary catheter for a short time.
Recovering in the hospital
You’ll stay in the hospital for about 3 to 7 days. Your stay may be longer or shorter. This will depend on your overall health and how fast you heal.
You may start rehabilitation, including physical therapy (PT), soon after surgery, depending on your health. The goal of rehab is to help you reach your best level of health and quality of life, and to support your independence in walking and daily activities. You will have a rehab healthcare team. This may include doctors, therapists, prosthetists, surgeons, nurses, and others involved in your care.
PT will help stretch and strengthen your muscles. It will also help prevent shortening of muscle or joint tightening. You’ll learn how to safely move between your bed and other surfaces, such as a chair. This helps prevent falls so that your healing wound is protected. Later, you may be able to move around using a walker or crutches, if your surgery was on a lower limb. You may work with an occupational therapist. They can help you resume tasks, such as showering and dressing.
Going home
You’ll be ready to go home when you are stable. And when your pain is controlled by pain pills. You’ll also need to be able to move safely between surfaces. If you’re having trouble with these tasks, you may need more help. This may mean going to a nursing center or a rehab unit, if your amputation was on the lower limb. If your surgery was on a lower limb, you may go home in a wheelchair. It may have a special platform called an amputee board to support your residual limb. You may need to arrange for help at home.
At home
At home, you’ll need to keep doing the exercises you were taught in the hospital. This will help prepare your residual limb to be fitted for a prosthesis. At all times, take care to move around safely to prevent falls. Falling can reopen your wound. Use your wheelchair, walker, or crutches at all times, if you get them.
Following up with the surgeon
You’ll need to follow up with the surgeon about 5 to 7 days after you go home. They will check how your wound is healing. The stitches or staples will likely come out about 2 to 3 weeks after surgery. This could be longer if you heal more slowly due to other health problems. Once healed, you may be able to be fitted for a prosthesis.
When to call your healthcare provider
Check your wound at home as directed by the surgeon. Call your healthcare provider right away if you have any of these problems:
-
Fever of 100.4º F ( 38.0°C) or higher, or as advised by your provider
-
Chills
-
Red streaks on the skin around the wound
-
Thick, cloudy, or yellow-brown drainage or odor from the wound
-
Skin that pulls apart at the wound
-
Severe increase in pain
-
Excessive bleeding